Understanding disease trajectory to guide precision policy, a case study in COPD
Understanding disease trajectory to guide precision policy, a case study in COPD
Abstract
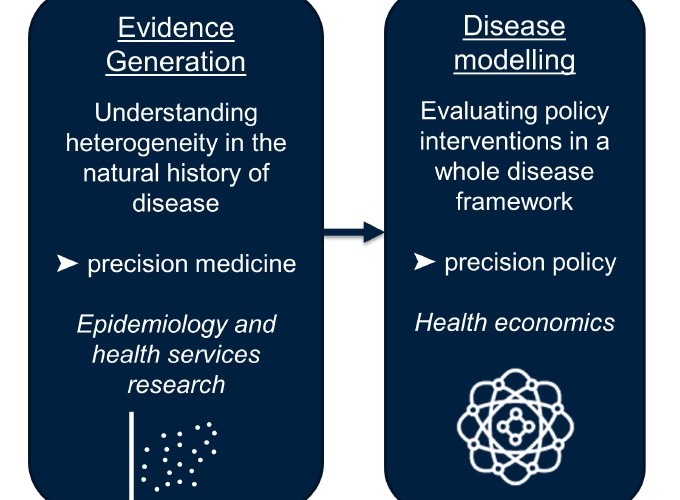
The highly anticipated paradigm shift from population-level to individual-level decision making in health care requires robust evidence on the distribution of risk factors, variations in patterns of care, and heterogeneity in disease outcomes. However in many cases, sufficient evidence to enable this paradigm shift does not exist. I will discuss this topic in the context of Chronic Obstructive Pulmonary Disease (COPD), which is one of the most common chronic diseases globally. In response to the ‘underdiagnosis epidemic’ in this disease, a one-size-fits all approach to screening is traditionally proposed. However, this approach has been shown to provide poor value for money. In order to develop a more efficient case detection strategy, I generated evidence on the extent of heterogeneity in various aspects of the natural history of COPD, as well as on patterns of care that give rise to opportunities for an earlier diagnosis. A ‘Whole Disease Model’ of COPD was used to incorporate this evidence and to fully explore the decision space created by a multitude of patient- and disease-related factors. This framework of evidence generation to understand disease trajectory, followed by whole disease modelling to evaluate policies can be transferred into the context of other chronic diseases and used to improve patient care.